It’s All About: Dysbiosis vs Symbiosis
A healthy gut is a partnership between microbes and the body as a whole.

When this relationship goes wrong — when the wrong microbes become dominant and “friendly flora” become weak — gut health stops serving the needs of the body. This is called dysbiosis and, while correctable, it creates a heavy burden on the body.

The goal is to move away from the trap of dysbiosis and progress toward symbiosis — where the gut microbes fully support the body’s health.
The solution is often not as simple as throwing supplements at the problem. That may help in less-intense situations, but gut health — and the microbes that affect it — is an intricate fabric, affected by nearly every aspect of our body and environment.
Therefore, overcoming poor gut health requires a long-term approach that includes supplements, sleep cycles, therapeutic light, movement, and environmental factors.
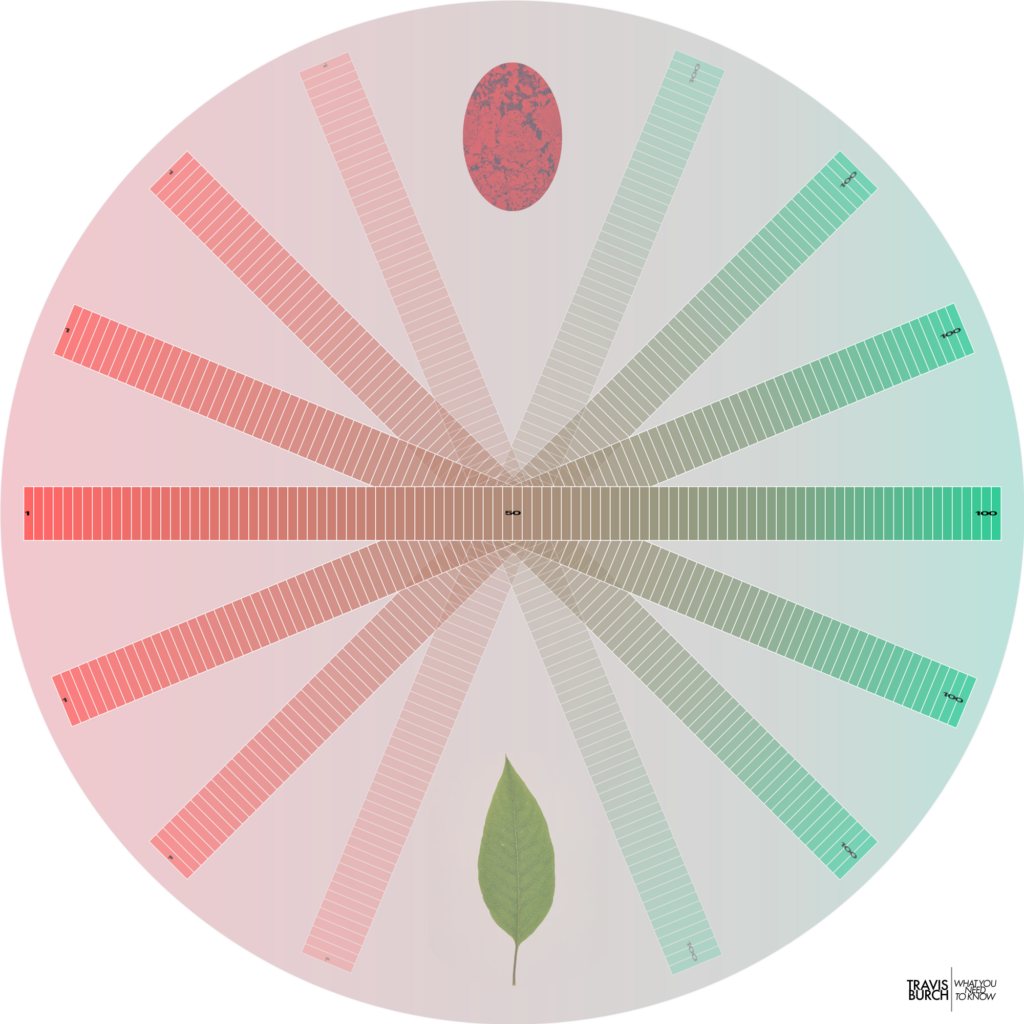
It’s Not Black & White: Your Gut Health is On a Spectrum
There aren’t just two options: “healthy” or “unhealthy.”
Instead, imagine a scale from 1 through 100. Perhaps your gut health is closer to an 80. Or maybe it’s a 40.
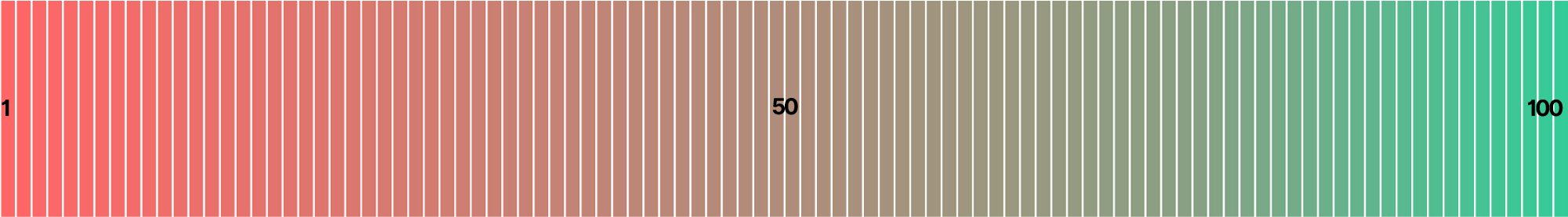
Very few people have perfect gut health — in fact, “perfect” may not exist!
Therefore, everyone can improve their gut health — through better foods, stress management, sleep, environments, and safe supplements.
There seem to be many, many ways for gut health to be healthy — along with endless ways for gut health to be bad.
The gut microbiome changes around the globe. There doesn’t appear to be any one, true way to great gut health.
There are endless pathogens — and combinations of them!
And there are endless combinations of healthy microbes, too.
Good gut health boils down to this: What’s your ratio of good microbes to bad?
Understand Gut Health
Microbes — bacteria & yeast — live in colonies, or biofilms.
These biofilms are essentially a slime, or sludge that provides protection from potential threats.
Biofilm forms when bacteria adhere to surfaces in moist environments by excreting a slimy, glue-like substance.
https://www.biofilm.montana.edu/biofilm-basics/what_are_biofilms.html
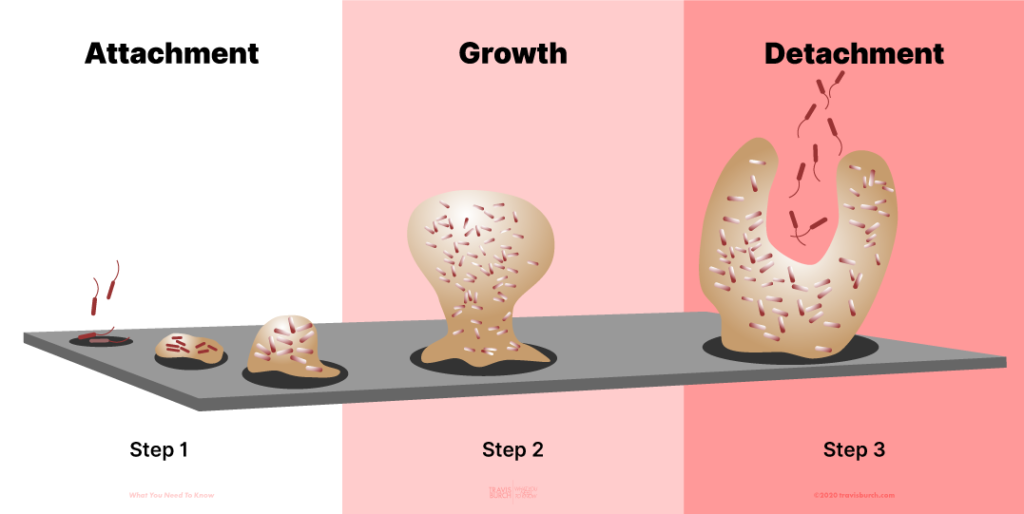
The Biofilm Lifecycle
A biofilm can contain one species, but usually is a mixture of many — often hundreds — of microbial species.
Biofilm facts:
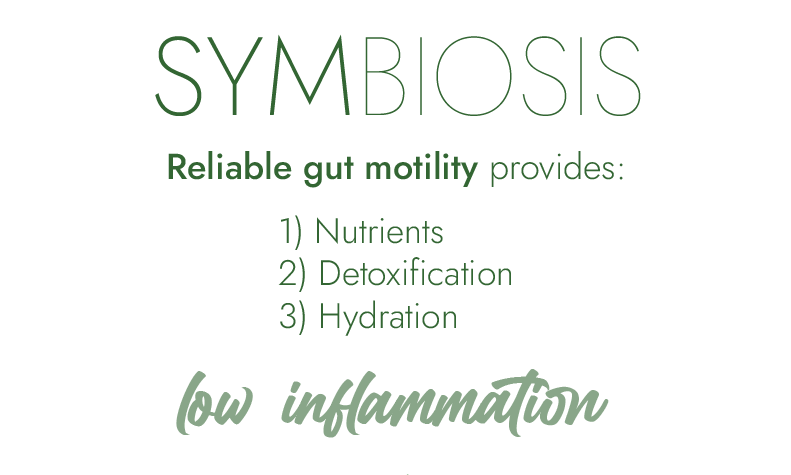
Symbiosis happens when gut microbes work together with the body.
Healthy, Balanced Flora
Symbiosis is when gut microbes are beneficial, working in concert with the body to 1) maintain immunity from pathogens, 2) digest food and supply nutrients, and 3) break down toxins in the gut.
Symbiosis defined: When greater than 80% of microbes are “good.”
SIGNS OF SYMBIOSIS
In symbiosis, people are able to:
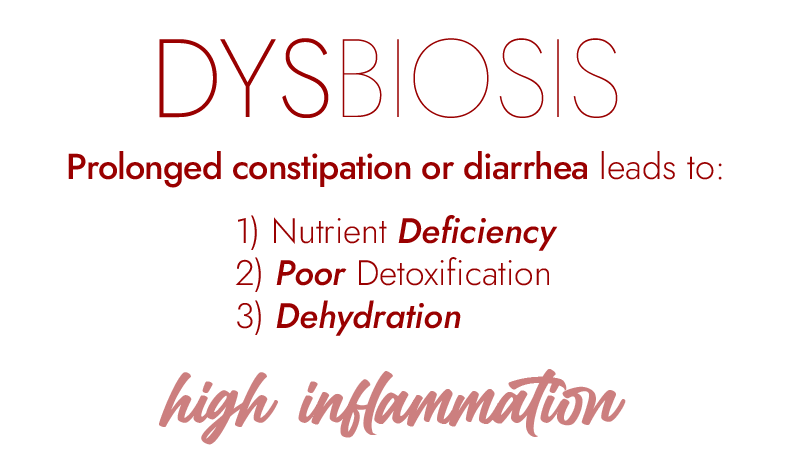
Dysbiosis is when the gut microbes begin to work against the body.
Unhealthy, Imbalanced Flora
Dysbiosis is when too many unhealthy microbes live in the gut. These bad “flora” release toxins (instead of helpful nutrients) when they digest our food and they don’t help our immunity. They can even release hormones that adversely affect our brains.
Dysbiosis defined: When less than 80% of microbes are “good.”
SIGNS OF DYSBIOSIS
A healthy gut microbiome is a champion for your health, particularly via these four functions.
Function #1
Nutrient Absorption
The intestines absorb nutrients from our food.
First, gut microbes help break down food for absorption.
Then, the microbes create extra nutrients as they break down (eat, or ferment) our food.
These nutrients — created by healthy gut flora — include copious amounts of B-Vitamins, Vitamin K, butyric acid, acetic acid, and propionic acid. All of these nutrients are essential for bodily health and resilience — and even the ongoing strength of your gut microbiome.
Function #2
Detoxification
The liver dumps its bile (with its toxins) into the intestines.
These toxins need to stay trapped in the intestines — not leak back into the bloodstream. With proper bowel movements and stool formation, these toxins will never stay too long in the gut. Instead they’ll always leave the body quickly.
Fiber is critical for this — absorbing and trapping liver toxins — so they can be excreted in the next bowel movement. Healthy stool formation requires a little fiber each day (and each meal, ideally) — and a strong gut tolerates fiber well.
Healthy microbes also break down toxins while in the gut, protecting the body further from toxicity.
Function #3
Immunity
Inside the intestines is outside the body.
When food is in the intestine, it has not entered the bloodstream yet.
On average, humans swallow over a trillion microbes per day (bacteria, fungus, or virus). Your gut’s job is to keep them out of your bloodstream, and keep them from becoming too comfortable while in the intestines.
How does the gut become hostile to microbes — and prevent them from growing too much? Enzymes, acids, and a healthy mucosal barrier (or lining). The mucosal barrier is quite literally — in scientific terminology — a slime.
Good Microbes Improve Hostility
Good bacteria release their own enzymes and acids, too, as part of their own defenses.
This helps fight off invading species in addition to the body’s immune defense.
The Gut Lining is Semi-Permeable
The gut lets good things into the bloodstream (food) and stops the bad things from entering (all microbes are stopped).
Therefore, your gut lining is “semi-permeable.” It selectively lets nutrients in, while keeping bugs out.
Microbes entering in the bloodstream is a very, very bad thing — an infection! This will cause lots of inflammation. A leaky gut can allow microbes into the gut, causing chronic immune reactions after meals.
This is why about 70% of the body’s immune cells are located in the gut — designed to keep all those microbes (healthy ones and pathogens, alike) out of the bloodstream, and inside the gut, where they can be handled.
Good Microbes Improve Immunity
“Good” microbes that reside in the gut help keep potential invaders at bay by boosting the host’s immunity. They also help keep the gut lining intact and tight — and not leaky.
When the gut is healthy, it is a formidable immune system against foreign microbes and pathogens. When it’s sick, it is a weak defense.
Function #4
Brain Chemistry
Research is showing that gut flora create chemicals and neurotransmitters that affect and control brain function: serotonin, butyrate, GABA, glutamate, and more.
The Gut-Brain Connection
Good and bad microbes directly produce or consume GABA and glutamate, affecting this delicate balance in the body’s neurotransmitters.
Good flora tend to create beneficial brain chemicals and stimulate the vagus nerve to communicate with the brain.
Bad flora tend to release chemicals that interfere with the communication between the gut and brain, increasing the likelihood of anxiety-like behavior.
The Four GUT Functions
In Symbiosis:
The four gut functions are working well.
In Dysbiosis:
The four gut functions are working poorly.
4
Causes of Dysbiosis
Chronic Stress
→ The brain needs rest, peace, and hope to be healthy.
Poor Diet
→ Artificial ingredients, junk foods, over-processed foods feed bad microbes.
Undereating
→ Promotes stress in the body, which harms gut balance.
Overeating
→ Overwhelms good microbes, and feeds bad ones.
→ Depletes body’s nutrients, which weakens gut immunity.
Restrictive Diets
→ All restrictive diets can weaken the gut by either 1) overfeeding certain microbes, or 2) weakening the body’s metabolic energy.
Exposure to Toxicity
→ Chemicals, mold, excessive fragrances, & sick buildings can expose the body to various toxins, which harms the gut.
Trauma
→ Injury, abuse, neglect, & chronic stress can systematically weaken all gut functions.
Sedentarism
→ Daily movement is essential for regularity and bile flow.
EMF
→ *Excessive* radiation from wireless pulses, fields from electronics can disrupt gut function in those who’ve become sensitized.
Infections
→ Infections sometimes migrate to the gut, and antibiotics used to treat them can harm the gut flora.
Antibiotics/NSAIDS
→ Antibiotics can wipe out all good flora.
It’s important to see how well a health gut works.
A healthy gut handles nutrients, toxins, & water with ease.
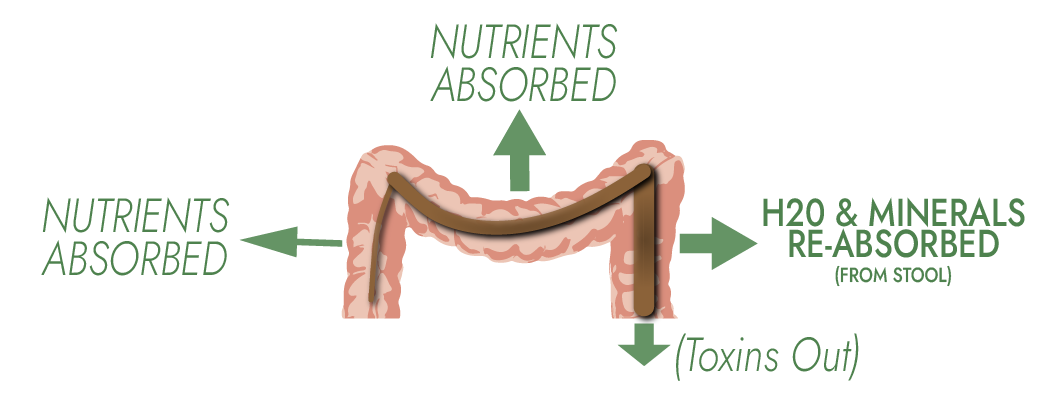
A healthy stool means that healthy microbes are growing and releasing nutrients:
Dietary fiber traps toxins inside the healthy stool — for excretion at your next bowel movement.
The lower colon reabsorbs water and minerals from stool, keeping the body hydrated.
Symbiosis Summary
- Nutrients are well-absorbed into body.
- Toxins stay trapped in stool → then exit body.
- Immunity stays high.
- Brain Chemicals are balanced, healthy.
Low Toxicity
+ High Immunity
= Low Inflammation
Adequate nutrient absorption = Good metabolism, strong immunity, solid detoxification.
The “Goldilocks Speed” Keeps Flora Healthy
A good motto for the gut: “not too fast, not too slow.”
One daily, well-formed stool is about right.
When food digests extremely well (and when coupled with a great circadian rhythm), bowel movements tend to even happen daily around the same time.
A river or stream needs moving water to stay fresh.
Regular, daily bowel movements allow healthy flora to thrive and prevent pathogens from becoming too comfortable.
A constipated gut handles nutrients, toxins, & water poorly.
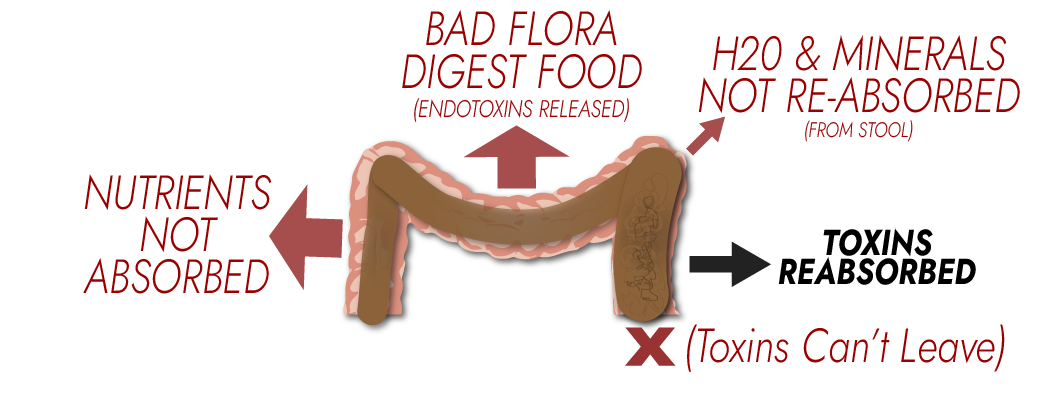
Stool is unhealthy & compacted.
- Good microbes aren’t present.
Bad microbes release endotoxins when they eat your food.
- Bad microbes release unhealthy hormones and neurotransmitters.
Toxins can’t leave the gut, and enter the blood stream.
- This causes a chronic immune reaction — inflammation — around the body.
Effects of Constipation
Summary
- Nutrients poorly absorbed into bloodstream..
- Toxins can’t leave → re-enter bloodstream.
- Immunity is weakened.
- Brain Chemicals are unhealthy, unbalanced.
High Toxicity
+ Low Immunity
= High Inflammation
Low nutrients = Low metabolism, low immunity
7
A gut with chronic diarrhea handles nutrients, toxins, & water poorly.
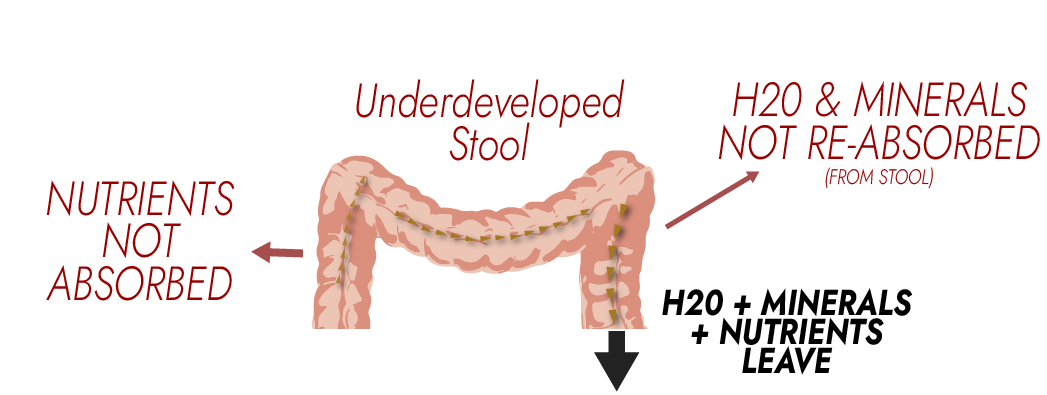
Stool cannot form.
- Good microbes can’t thrive.
Your food is not properly digested and broken down.
- Nutrients aren’t absorbed
- Water and minerals are lost.
A weak microbiome allows pathogens — bad bugs — to become strong.
- Bad microbes release endotoxins when fed.
- Bad microbes release unhealthy hormones and neurotransmitters.
Effects of Diarrhea
Summary
- Nutrients – little opportunity for absorption.
- Toxins – poorly trapped by healthy stool → will re-enter bloodstream.
- Immunity — No robust gut microbiome to protect against pathogens.
- Brain Chemistry + Neurotransmitters are poorly unbalanced.
High Toxicity
+ Low Immunity
= High Inflammation
Low nutrients = Low metabolism, low immunity
Any microbe — bacteria, yeast, fungus — can rapidly grow and reproduce.
Speed Demons –>
Microbes only need food and water (and a surface) to grow. The gut is perfect for this: we constantly eat and drink.
When food feeds the flora that lines your intestine, the flora can double in numbers in well under an hour. A microbe’s environment greatly determines its rate of growth.
Consider that up to 60% of your stool is this flora, which grows as it eats the food you eat.
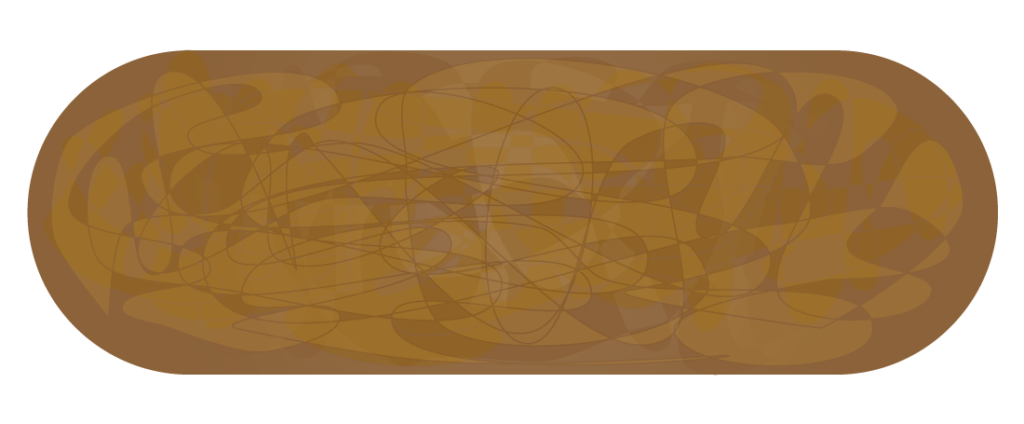
60% of the stool is microbial life: bacteria and yeasts.
Visualize how healthy stool is formed:
- Good flora eats your food,
- Flora grows (doubles) rapidly,
- You now have fresh bulk to slide easily through the GI tract.
This new bulk is largely colonies of microbes — especially fermenting fibrous and starchy foods, and releasing nutrients (like Vitamin K1+2, butyric acid, & B-Vitamins) or endotoxins (from bad flora).
The Risk
Unfortunately, bad microbes, when they are present, can double and grow just as fast.
This is often what’s happening when someone feels poorly after eating: Bad microbes grow and metabolize the meal, releasing endotoxins and causing an immune response.
9
The Immune System
& the Gut
The lining of the intestines is the most important interface with the outside world.
The gut lining must decide what gets into the body and what stays outside. Only one thing should get into the body: Nutrients.
Around 70% of the immune system is located in the gut — and for good reason.
Incredible Surface Area
Designed to maximize the absorption of nutrients, the gut lining has 150X more surface area than the skin. That’s as much surface area as a tennis court.
This presents a challenge, though. The high surface area creates lots of potential entry points for pathogens — and nearly endless gates to guard.
Each of the body’s surfaces are designed to keep the outer world exclusively on the outside.
=
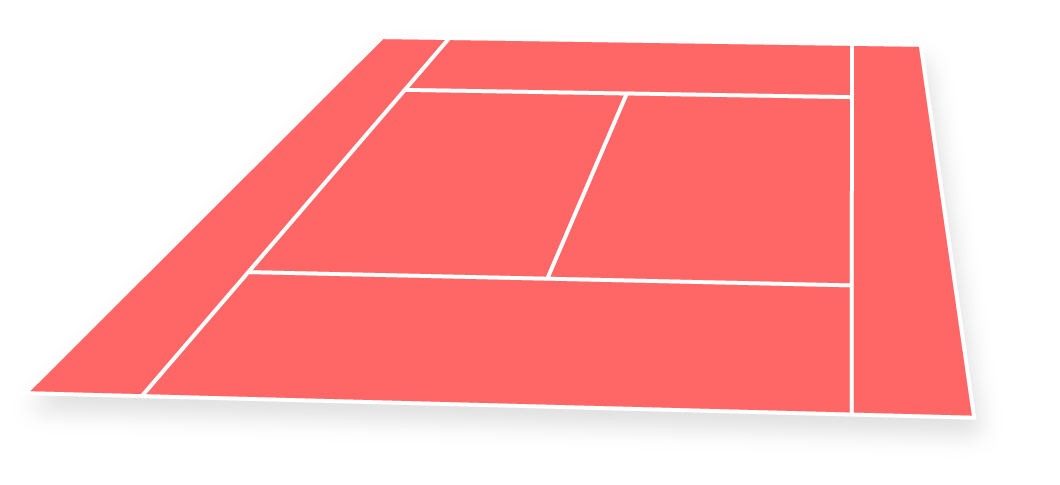
Yet, the gut lining is teeming with microbial life — a thick biofilm of microscopic bugs. Imagine a tennis court covered in microbial biofilm.
In good health (symbiosis), this slime helps digest food and protect against invading pathogens.
In dysbiosis, the slime is actively poisoning the body, causing poor digestion of food, and preventing nutrient absorption. It causes ongoing inflammation.
The digestive tract is a warm, moist place where fermentable foodstuffs constantly enter — and then reside.
The body’s immune system must be strong to keep the hostile microbes at bay.
The Immune System Resides In The Gut
The immune system is so heavily concentrated in the gut: A premier threat to all animals is that the gut becomes inhabited with bad actors — bad microbes.
Microbiota signaling to the immune system plays an important role in preparing the body for potential pathogen infection.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721637/
Infants Receive Mother’s Immunity
Babies are born with virtually zero gut microbiome.
However, nature has a strategy to meet this challenge: A mother’s first milk (colostrum) lets a baby benefit from the mother’s immunity as the infant’s own immunity and microbiome develop.

When gut health and immunity is weak, the human digestive system makes for an excellent breeding ground for pathogens.
Inside the intestines is still “outside” the body.
The intestines decide what to allow into your bloodstream.
It takes a strong immune system to keep the gut clear of pathogens.
Territory is everything for microbial organisms. That’s why microbes are quite ready to fight for their turf — against other microbes.
Dormancy is what happens when conditions aren’t suited for a microbe to thrive.
Microbes tend to go dormant when:
Small Numbers vs Big Numbers
When species numbers grow, the species will become more aggressive– attacking other species for territory in the gut.
When their numbers dwindle, species begin to become dormant, and less hostile to their neighbors and their human host.

Microbes “fight” other microbes by releasing harmful chemicals, enzymes, and sometimes by outright consuming other species.
“Bad” microbes will fight good microbes, to gain dominance and vice versa. Pathogens release endotoxins when they eat your food.
Good microbes — already present in a healthy gut — will also “fight back” against bad flora, to maintain dominance.
When food enters the digestive tract, healthy microbes release nutrients.
Dysbiosis is involved in most disease states, including aging.
Our microbiota and health develop (and age) hand-in-hand.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004897/
In Dysbiosis, All Gut Functions Can Be Compromised
A restrictive diet can relieve symptoms.
However, restrictive diets often cause their own issues over time — as a result of avoiding foods.
Imbalances occur in vitamin and mineral intake. Food avoidance can lead to intolerance of the absent foods. Too much or too little of any food can result in negative changes to the microbiome.
This results in diets bouncing back and forth — perpetually looking for what will give them relief of symptoms or an improvement in energy.
The Long Term
Restrictive diets are rarely a long-term solution.
They are, instead, a band-aid — sometimes giving the body a break from the constant tidal wave of endotoxin, constipation, maldigestion, or other symptoms.

Unfortunately, the root causes that cause digestive and health issues almost certainly continue to exist, and the symptoms can only be avoided by maintaining the diet.
More And More Restriction
Diets frequently become increasingly restrictive over time.
As a first restrictive diet seems to ‘wear off,’ more and more foods are removed to try and achieve the same relief. It can even be difficult to ever reintroduce a food once removed, if only because of the psychological hurdle developed by negative beliefs about previously-avoided foods. The gut flora changes in response to the diet, too. Removing a food can shift the microbiome to a state where certain foods less well digested.
The cure to our digestive problems may not be as simple as removing foods.
After all, restrictive diets can make food intolerances worse. Foods that were once acceptable become less tolerable over time as the gut microbiome changes during restriction.
Restriction: A Necessary First Step?
There is certainly a place for limited diets.
Dietary restrictions might be a necessary first step to stop feeding the bad flora.
Why? Because it certainly doesn’t make sense to continue eating foods that cause inflammation or an immune response.
However, to avoid the trap of eternal restrictive dieting, gut health must improve so that diverse foods are tolerable and even welcome in the diet.

Any time food is eaten, bad microbes are capable of digesting food and releasing toxic metabolic byproducts.
These toxic byproducts cause inflammation and immune response. In poor gut health, the gut barrier is weak, meaning more toxins enter the bloodstream. Even microbes enter the bloodstream, causing even more inflammation.
Endotoxin
In dysbiosis, food gets “eaten” by bad microbes.
Instead of releasing nutrients (like good flora do), these pathogens release toxins into the gut, which are absorbed into the bloodstream.
In the bloodstream, endotoxin causes inflammation harms tissues and organs. In dysbiosis, this happens every time food is eaten.
…Detoxified By the Liver
These endotoxins must be removed by the liver.
Over time, the liver becomes overburdened and sluggish, resulting in poor detoxification in the body.
Ever-rising bodily toxicity causes gut health to worsen further. Good gut flora suffers and bad flora happily take their place in a vicious cycle.
As gut health worsens, the ability to properly absorb food diminishes, leading to energy deficits and nutrient deficiencies, which may be mild enough to be subclinical — yet strong enough to affect the way someone feels and their long-term health outcomes.
As immunity drops, the body’s viral and pathogenic load often increases, complicating things further and possibly leading to a chronically activated immune system (and more inflammation).
What’s more, the brain chemicals released by bad flora can lead to chronically elevated serotonin, general depressive feelings, and brain fog.
Endotoxins Can Be Debilitating
Healthy habits, foods, and thoughts may not be enough to restore vitality when gut microbes are poisoning the body continuously after every meal.
The Story Of Dysbiosis
Is one of
high toxicity,
high inflammation,
low nutrient absorption,
& poor brain chemistry.
My view of fasting: Many of the benefits of fasting (as well as low-carb, carnivore, and vegan dieting) are largely the result of less endotoxin production in the gut. What helps more, a few days without needed nutrition — or a few days’ reprieve from a toxic onslaught?
Of course, we can’t fast indefinitely — meaning fasting is not a long-term solution to gut problems.
To restore symbiosis in the gut reduces the endotoxin load throughout the body.
Symbiosis, therefore, means less endotoxin — which means less inflammation — throghout the body.
It is not surprising that a small dose of E. coli LPS [endotoxin], injected directly into the bloodstream, can elicit fever and other responses in volunteers.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5014740/
When the gut microbiome becomes more healthy, less endotoxin enters the bloodstream.
Symbiosis Can Be Restored
When at my worst (for several years), nearly every food used to cause heavy inflammation.
Things got so bad, to avoid symptoms, I could only eat fresh-pressed vegetable juices.
Now, I eat essentially any food group and feel no rise in inflammation.
And of course, “leaky gut” can play a role here, too — especially when talking about endotoxin.
The truth is, the science surrounding the “leaky gut” is absolutely in its infancy.
A leaky gut is a phenomenon where the gut membrane is weakend — causing it to fail to perform its two primary tasks:
- letting in nutrients into the bloodstream
- while keeping pathogens out
When the gut lining weakens, it lets everything into the body indiscriminately — particularly undigested food and microbes.
This is troublesome because undigested food and microbes cause an ongoing immune and inflammatory response that over time damages tissues and restricts metabolism.
The main theory is that bad microbes cause this: they set up colonies that burrow into the gut wall and eventually burst through.
Other theories suggest that the tissues can’t maintain integrity simply due to lack of energy supply as the body weakens.
The reality could be an “all of the above” situation.
The gut’s permeability is always variable (for instance, permeability increases 80% after exercise). With leaky gut syndrome, permeability is chronically increased.
The leaky gut theory is linked to autoimmunity and food intolerances, as well.
A leaky gut can heal over time! Mine certainly did, along with all of the typical symptoms.
Virtually every aspect of gut health is controlled and impacted by the circadian rhythm.
Gut health simply cannot escape the grasp of the circadian rhythm.
The circadian clock in the intestine works in close connection with gut microbiota.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721637/

Therefore, your circadian rhythm is a close partner with your gut health:
The GI tract… operates on a ~24-hour circadian schedule that anticipates — and prepares for — changes in the physical environment associated with day and night.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721637/
And if that schedule is off? Not synchronized with the sun (solar time)?
- Your gut function may not be optimized.
- Your gut is not able to “anticipate and prepare for what happens throughout the day and night”.
The proper way to look at this:
The circadian rhythm — your sleep hygiene — is an incredible opportunity to improve your gut health.
Remember the gut’s functions throughout the day and night:
Each of these gut functions is optimized via alignment of the circadian rhythm.
Your gut microbiome’s activities — and its microbial makeup — change throughout the day.
1) Time of day influences human susceptibility to enteric pathogens, 2) circadian disruption lowers human resistance to enteric pathogens, 3) jet lag — not just differences in sanitation and hygiene — is a risk factor for traveler’s diarrhea.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721637/
Who’s in Charge: Gut or Sleep?
Between the gut and the circadian rhythm — which one leads?
It is clearly — and scientifically proven — that the gut microbiome and the circadian rhythm exist in a “bi-directional relationship”:
Moreover, the abundance, composition, and function of gut microbiota are dramatically altered in circadian [disruption], further indicating a bi-directional relationship between circadian rhythms and the gut microbiome.
…Dysregulation of circadian function due to shift work, or perturbed microbiota signaling in the gut, might therefore have drastic effects on the level of inflammation within the GI tract.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721637/
Bring your gut health into balance — improve your circadian rhythm.
Congratulations! You’ve completed ‘Why the Gut?’
My gut health was extremely poor ever since I was young. My parents have shared stories of my gastric troubles even as a very small child.
As such, focusing on my gut health has revolutionized my life.
Restoring my gut microbiome play an integral role in healing my chronic health issues. In fact, it has even launched me further — into new levels of my own health that exceeded my own anticipation. My digestion is, quite literally, the best it’s ever been in my life.
Two Very Important Points
Two major steps to improve the gut microbiome are:
1) Identify the supplements that helped.
2) Keep doing the ones that work.
The essential principles discussed in this Gut section — such as: repopulaton versus antimicrobials, supplement timing, and more — were all subserviant to those two concepts: identify helpful supplements and remembering them after you see improvement.
I find it helpful to keep a fresh, light approach. When you find a great supplement, believe it is helping you. If something feels burdensome, there might be a reason — trust that feeling. It’s okay to look elsewhere, to give yourself a break.
Some of us had poor gut health when young. Others developed poor gut health as adults — after various health challenges.
Maybe it was too many rounds of antibiotics. Maybe it was chronic stress or trauma. Perhaps it was a sick building, or chronically disrupted sleep.

Knowing the root cause could help. But, amazingly, it often doesn’t matter! What’s best, is to know one thing: It seems like a good idea to improve my gut health.
Merely following protocols may not be the answer, though. Actually, it’s usually not the answer.
Why? Because there’s a lot of (bad) information out there. So much confusing information. There are endless, high-priced, overconfident practitioners (qualified and unqualified) who can lead you down paths that will mostly waste your time. Most will teach you rules you’d do well to forget.
There’s no one thing you have to do to fix your gut.
You’re not stuck. There’s not one path. You don’t have to figure it out like a computer.
The best approach is a playful, free one. Try things and see what works. Let go of what doesn’t serve you.
Remember those two concepts:

Identify what seems to help.
And if something really helps, remember it!
We all do this: We find something helpful, improve some, and then stop doing what got us there (often because we start to feel better). When we stop the habit, we’ll often slowly lose some progress — and forget the habit altogether, even though it really did help.
Information overload (especially from online gurus) contributes to this! We can lose sight of what we know has helped us in the past.
You’re not stuck. You are not trapped. Your health can change, and your life can change!
Your progress comes, not by sheer force of effort and knowledge, but through a sense of ease. Trusting your intuition and your body, listening for its messages, and combining this guidance with only the smartest and wisest gut health principles.
Sometimes we aren’t meant to leap out of our situation immediately. Maybe there are things we need to learn and master right here — right where we are — so that when the leap is made, we’re ready for it. We can make our newfound health permanent, and sustainable.
Where are you on the gut health spectrum?
What have you already learned about yourself? Perhaps it’s how to eat foods you actually tolerate instead of rigid diets? Perhaps it’s the best gut supplements for you — rather than what someone else says to take?
I did recover my health — and my gut health continues to improve to this day, years later! More than a decade after working out my own approach to healing, my health and my life keep rising higher.
I believe in you!