Persistent poor sleep can feel like a prison.

You just want relief from being awake.
“Why can’t I fall asleep? What’s wrong with me?”
Sometimes, a sleep supplement solves the problem — until the body builds tolerance and becomes resistant to it.
The body creates new cells that have fewer chemical receptors for the supplement’s active compound that induces sleep.
However, sleep shouldn’t need to be induced. If we are looking to induce sleep, we’re probably only thinking in the short-term.
And short-term thinking doesn’t sustainably solve the problem of chronic insomnia.
Sleep is a natural process, one that we can trust our body for every single night.
That is, unless we are making big mistakes regarding our health.
Perhaps in your situation, it’s the unnatural stuff — or even the unnatural way we do/take natural things — that prevents the body from being able to sleep.
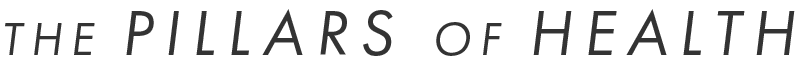
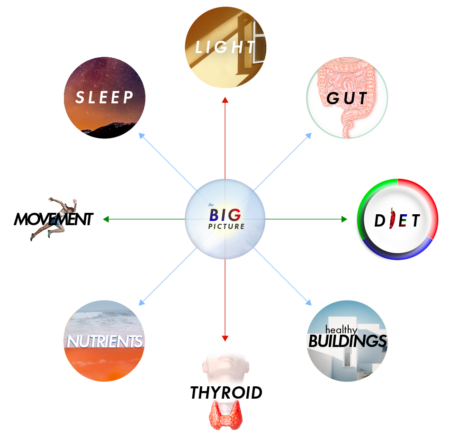
Get to the Root Cause
Certainly, anxiety about insomnia can make the situation worse.
That’s why it’s so important to understand what is at the root cause of poor sleep.
When we grasp the pillars of excellent sleep, and know to avoid big mistakes, we can find confidence that great sleep will be ours. Every single night.
There’s less room for anxiety about sleep if we have a deep understanding of our body — what works for us and the general factors that improve or harm sleep.
If you find yourself struggling with insomnia, look at this list of potential causes. If you recognize something on this list, you may have identified a potential cause of your insomnia. Which means it can be fixed holistically.
Let’s reduce anxiety about sleep — and find solutions that work, long-term.
Among the unwell, a premier contributor to insomnia is sleeping-in.
Sleeping-in throws off the circadian rhythm so deeply that, without doing anything else “wrong,” falling asleep at night can become extremely difficult.
Some folks are able to overcome the negative impact of sleeping-in by being extremely active during the day — healthy athletic types and performers can sometimes appear to “get away with” a later circadian rhythm. These people are typically younger and haven’t faced a scourge of debilitating health problems, while sometimes living on the high of sheer exhaustion. They may be able to “pass out” at night, but this is no recipe to maintain health, much less restore it.
For the rest of us who have struggled with health issues, sleeping-in greatly disrupts your ability to fall and stay asleep the next night. The circadian rhythm is delayed, which means melatonin won’t rise properly the next evening.
Sleeping in also causes you to miss out on the serotonin created by morning light. Without this light stimulus, evening melatonin will not be adequately created from the early-produced serotonin.
For those folks interested in the ill effects of high serotonin, perhaps the most reasonable way to fight back (besides improving gut health) is bright sunlight — which balances serotonin by raising dopamine during the day and lowers serotonin at night by properly converting it to melatonin.

Insulin sensitivity (a marker of diabetes) is also impaired by sleeping-in, which could directly lead to a metabolic energy deficit at night. Needing to eat late at night to induce sleep, or waking up hungry? Sleeping in could be impairing your glucose metabolism all day, destabilizing your blood sugar, and making it harder to stay asleep through the night.
Staying-up late at night is the evil twin sister of sleeping-in, contributing to future insomnia, and making more sleeping-in likely. Late nights also allow bright light at night (which is correlated with nearly every disease risk factor) — making sleep less efficient, and further impairing an early rise the next morning.
When staying up late for any reason, protect your eyes from bright, blue light. It’s still best to follow natural light cycles to some extent. Better light cycles will disrupt hormones less, and make it more easy to get back on track after a late night.
If sleeping in has become the norm, the answer is to simply wake up early while supporting this change with simple circadian hygiene steps.
When shifting to earlier mornings, it will be necessary to endure one or multiple short nights of sleep. The days following short nights of sleep don’t have to miserable. The beauty of being awake early, even if tired, can shine through the temporary challenge of resetting the circadian rhythm.
Again, when coupled with other pro-circadian habits — proper light cycles, daily movement, meal timing, etc — forcing an early rise can invite exhaustion and “sleep pressure.” This sleep pressure, when coupled with better circadian habits can lead to an excellent reset of the circadian rhythm after long periods of sleeping in.
These tenets of good sleep hygiene — waking up early, being active, eating on time, and moving a little — are incredibly effective at restoring sleep in their own right and represent the solution to the type of insomnia that occurs as a result of sleeping in.
If powerful sleep hygiene methods do not succeed in enabling sleep, you might have another, deeper problem preventing your rest. Let’s explore further.
Nutrient imbalances are becoming exceedingly common in the modern health world — especially in those dedicated to boosting metabolism, hormone production/manipulation, and excessive detoxification.
Nearly every substance and chemical on the planet has some sort of metabolic effect.
Very little research is required to find endless lists of biochemicals, vitamins, and hormones that research suggests will boost — or inhibit — any particular biological activity.
Unfortunately, this approach of supplementation — to take vitamins and supplements for their drug-like effect — may be pyrite, or fool’s gold.
While a young and healthy person may be able to take hormones and nutrients without immediate, apparent harm — for instance, a college-aged fitness enthusiast taking steroids, stimulants, estrogen blockers, or high doses of nutrients to increase lean muscle and burn fat — for folks who aren’t already extremely healthy this approach can be a disaster, and sleep is often where the negative symptomology is ultimately displayed.
For folks who have been battling chronic illness for several years, this “metabolic boosting” and “hormonal manipulation” can lead directly to a no man’s land of severe insomnia with no clear path out of it.
Supplemental hormones can deplete nutrients, leading to deficiency of minerals and vitamins.
Hormone-blockers can lead to initial scarcity of certain hormones — only to then cause the body to create new cells that are hypersensitive to the hormone being blocked. This is especially common with estrogen-blocking supplements like DIM and calcium d-glutarate, along with cortisol blockers like Seriphos (and cortisol-lowering herbs, to a lesser extent).
Over time, supplemental vitamins and minerals — especially in isolation — can cause severe nutritional imbalances, particularly when focusing on boosting desired biological results.
Nutrients should rarely or never be taken for their drug-like effect — whether it’s to induce sleep, alter the metabolism, nudge hormone balance, or elevate performance — especially not long-term or in doses that far exceed 100-200% of the recommended daily value.

The fat-soluble vitamins (D, A, E & K) are especially known to cause sleep disturbances when levels are imbalanced or too high in the system.
The fat-solubles are incredibly powerful at boosting the immune system (they are quite antimicrobial) and are equally pro-metabolic. This means they are essential for health. It also means they can produce excellent results upon initial supplementation — with a happy honeymoon period of solid results — only to be followed by worsening symptoms that persist for weeks or months after the nutrient supplementation ceases.
When Vitamin D levels have become too high, it may even be necessary to avoid UVB light frequencies from the sun (from midday, summer light) until Vitamin D levels can return to a healthy level.
Vitamin A is a double-edged sword, much like Vitamin D. Much of the population will be deficient in both D & A, and yet some will be dangerously high in one or both (usually after supplementation). If one is low, that deficiency alone can wreck sleep. If one is high, that excess (or “vitamin toxicity”) can equally disrupt sleep.
Vitamin A & Vitamin D are just as likely to ruin sleep in excess as they are to restore sleep in deficiency.
Additionally, of particular importance is one’s sodium and potassium balance.
In chronic illness and hypothyroidism, sodium levels are often depleted, so adequate daily sodium intake can be incredibly pertinent for sleep. Any nutrient — when too low or too high — will raise levels of cortisol, and this is true of sodium in particular as a primary electrolyte.
Many folks will need to restrict sodium intake — and balance it with potassium.
Monitor this critical, fragile ratio daily, doubly-so if insomnia is a recurring issue.
For example, restless leg syndrome (RLS) is especially related to sodium/potassium balance. RLS is also linked to Vitamin D/A balance, as well as calcium/magnesium balance and iron levels. If any nutrient is low or high, restless legs can present — and extreme supplementation easily and often leads to imbalance.
All in all, any nutrient, when out of balance with its cofactors (read: all other nutrients), can cause persistent insomnia until supplementation has stopped and the body can balance itself once again.
It can take weeks for sleep to return when nutrients and hormones have been thrown out of whack, though improvements can often be noticed within mere nights of stopping the offensive supplementation.
In more severe cases of supplementation-induced imbalance, it may take active rebalancing to restore sleep in a timely manner.
Insomnia can certainly be caused when too-few calories are eaten –or– when enough calories are eaten too late in the day.
Glucose tolerance is lower at night and higher in the morning.
https://onlinelibrary.wiley.com/doi/abs/10.1111/dom.13391
When calories aren’t eaten early, they are less efficiently metabolize later in the day — leading to an energy deficit that can only be ameliorated by further, excessive caloric intake.
Simply put, eating too little, early, means even more calories must be eaten later in the day to compensate. The energy requirements of the body must be met, and if not early, your body will get them later.
Remember: Eating later in the day is very bad for health and, in particular, your circadian rhythm.
In cases of chronic illness (due to extreme dieting, infections, or even poor gut health), the body is in a perpetual state of energetic deficit.
In the low-energy state, adequate caloric intake is essential to facilitate sleep.

Erratic blood sugar (possibly as a result of a disrupted circadian rhythm or low-grade infection) can directly cause insomnia, too. Eating calories late is dysregulates blood sugar with remarkable prowess.
Therefore, when blood sugar regulation is a concern, it’s increasingly important to 1) eat enough calories and 2) eat those calories on time — early — and not late.
The popular notion that caloric restriction is a path to longevity can directly lead to insomnia. (Insomnia is not good for longevity).
However, the fact that eating late isn’t ideal doesn’t mean you should starve yourself during bouts of insomnia. If you find yourself unable to sleep due to insufficient daytime caloric intake — there’s no other choice but to get up and eat sufficient calories to allow for proper sleep.
Snacking at night certainly isn’t ideal (poor glucose metabolism, eating signals “daytime” to the brain, bad for gut health), but insomnia is clearly a worse outcome. When necessary, eat what’s needed for the night, and get back on track in the morning and the days that follow.
Daily movement is a major component of dependable sleep.
How? Movement reinforces the circadian rhythm by suppressing melatonin — and signaling daytime to the brain’s clock (suprachiasmatic nucleus).
The brain needs strong, powerful signals of daytime — each and every day — to keep the circadian rhythm intact. Movement, along with bright light and early meals, does that.
Movement reduces glutamate stores, allowing for a more appropriate GABA-glutamate balance in the evening which facilitates better relaxation of the nervous system.

Exercise also improves liver bile flow and digestive wellness, allowing for more efficient absorption of nutrients and, therefore, improved metabolic function — all of which support deep rest.
The lymph system is nourished by daily exercise and, when sleep cycles have been impaired, the lymph system depends upon movement even more deeply to clear lymph and the toxins housed inside it. This increased reliance on movement is because the circadian rhythm is critical for lymph function. In circadian disruption, movement is all that remains to stimulate lymph flow (along with, potentially, manual lymph drainage, massage and infrared light).
Some well-intentioned — but ultimately, misguided — health advice recommends extreme avoidance of exercise. While this advice is based on some measure of truth (long-term overexertion can harm health), we mustn’t ignore the fact that daily, tolerable levels of movement are absolutely critical to GI motility, lymph drainage, and, ultimately, preventing insomnia.
Hydration is a major challenge in chronic illness.
Bodily homeostasis and fluid balance often strugge due to chronic inflammation and poor nutrient absorption. Poor gut health and overburdened liver/kidneys are often factors, as well.
Monitoring fluid intake — as well as water quality — is important when sleep is a challenge.
There’s certainly a “Goldilocks zone” for each person when it comes to fluid intake.

The amount of water required will vary depending on the diet and intake of minerals.
Sunlight, light therapy, heat therapy, exercise, and mineral intake will all greatly increase daily water needs.
However, in hypothyroidism, it’s common for folks to restrict water intake and increase sodium consumption. This improves fluid balance caused by to hyponatremia (low sodium levels) as a result of various health challenges: low hormone levels, high inflammation, poor gut health, and poor nutrient absorption.
Increasing your sodium-to-water ratio may help sleep in those with hypothyroidism who waste salt.
Because sodium can calm the stress response and help keep blood sugar up, it’s common for hypothyroid folks to take a little salt on their tongue during nightly wakeups.
Keep in mind that it’s possible to go too far in either direction: both too much water or too much salt can be problematic. You need to find your own balance, and then remember that your needs will change as you become more healthy.
Ultimately, needing to manage water/mineral intake is a sign of severe fluid imbalance — the body simply is not maintaining homeostasis.
Frequent night urination can signal many things: diabetes, mold toxicity, high EMF exposure, and high inflammation. The root causes of fragile fluid balance need to be addressed going forward, rather than merely addressed through intense sodium/water balancing.
Poor gut health can cause each bite of food to stimulate endotoxin in the gut.
Endotoxin — in its own right — is a major disrupter of sleep.
Pathogens, when they become too comfortable in the gut, eat your food and cause inflammation. They’ll even enter the bloodstream — a place they certainly don’t belong — and trigger a strong immune response (more inflammation).
All of this inflammation disrupts cellular absorption of nutrients and metabolism — creating the scenario we discussed earlier, where the body cannot maintain its homeostasis.
Sleep become impossible when the body cannot maintain its own balance.
Some folks are able to find some temporary, spotty relief by removing problematic foods from the diet (such as grains, fibers, or animal products). However, this will not totally address the underlying health problems and may even cause deeper imbalances over time. Imbalanced diets tend to promote imbalance in the body.
If insomnia is truly persistent, it’s certainly possible gut health is a root-cause factor.
Of course, the circadian rhythm has a primary impact on overall gut health. Therefore, attacking both your gut and sleep simultaneously through strong sleep hygiene and a wise gut health regimen may present an uniquely effective approach.
Sick Buildings
If you’re really struggling with insomnia — and absolutely nothing else is helping — I recommend exploring the possibility that you’re dealing with a sick building.
When water intrusion or leaks cause significant mold growth — or air conditioning units go unmaintained and grow mold — this, alone, can cause insomnia all by itself.
Mold releases toxins called mycotoxins which directly cause inflammation. Spores can be allergenic and even become lodged in the mouth and nose and grow fungal colonies (possibly the gut, too). The scent of mold (technically “volatile organic compounds” or VOCs) is particularly disruptive to the sensitive body, too.
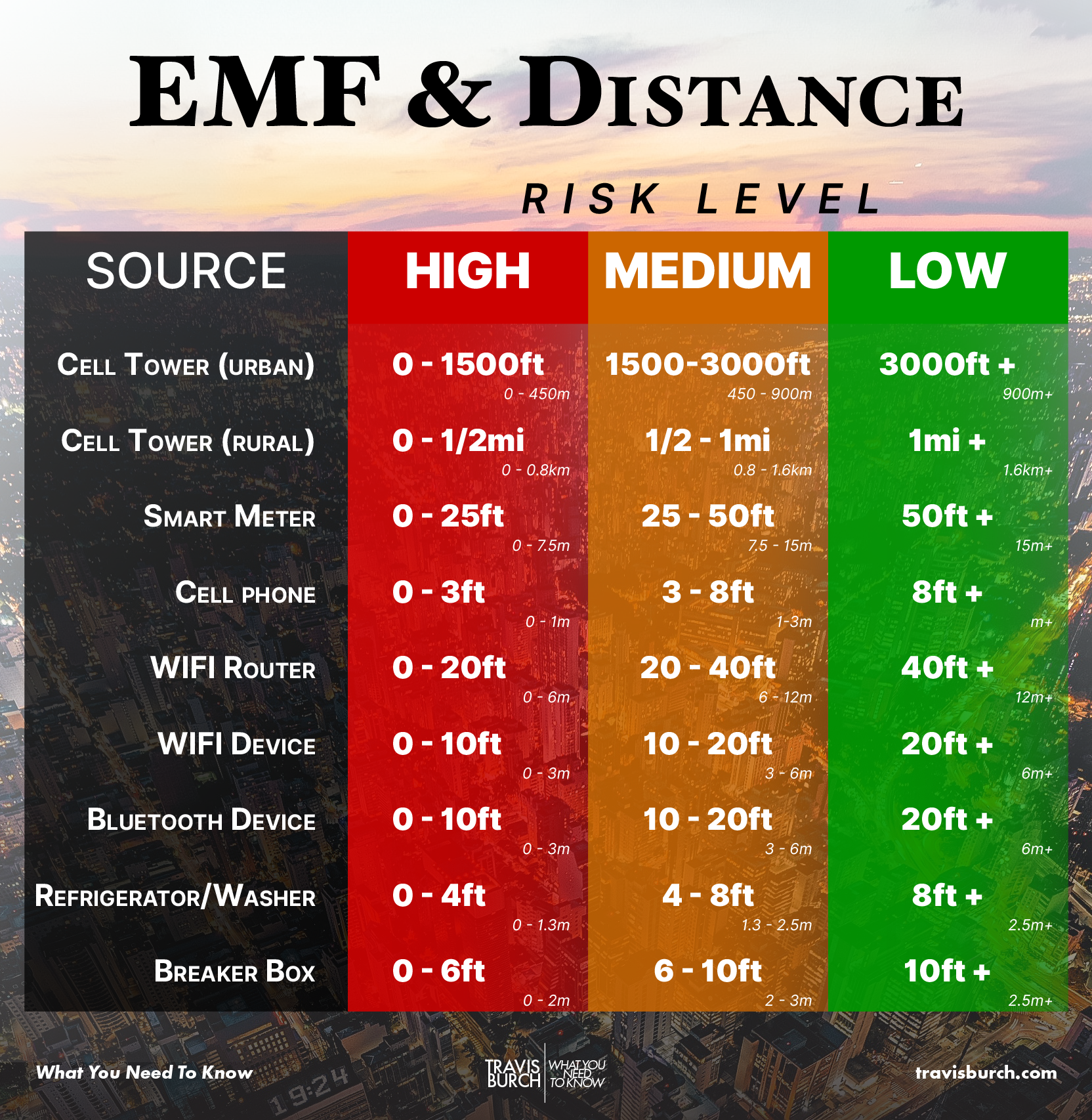
EMF, on the other hand, doesn’t affect everyone equally — but if you are senstivite it can cause sleep to flatline on its own, as well. EMF sensitivity typically co-presents with chemicals sensitivities, but not always.
Get to know your sleeping domain — is it within high-risk distances for any of the EMF-emitting sources in this chart?
It’s a never-ending process to understanding mold and EMF in the environment.
Mold is becoming a modern epidemic. Buildings are built with cheaper materials and tighter envelopes (less air exchange), and are inhabited by people who are too busy, ignorant, or financially limited to properly maintain the premises. Old houses are exposed to decades of potential problems, while new houses succomb to mold at the first sign of moisture intrusion — which can be common as construction mistakes are rampant.
EMF exposure is rising exponentially, with current average exposure levels most likely exceeding previous decades’ average exposure levels on a magnitude of millions of times more radiation — and that’s just the wireless component of EMF, not magnetic and electric fields, which may have remained more constant. One thing is for certain: EMFs are biologically active and not completely inert.
If you’re struggling with insomnia, it’s most important to understand why it’s happening — rather than look for a quick fix.
As tempting as it is to find a quick solution — and as sweet a relief a few decent hours of sleep might be — in the long run, the only thing worse than having insomnia now is still having chronic insomnia in the distant future.
That might be worth repeating:
In the long run, the only thing worse than having insomnia now is still having chronic insomnia in the distant future.
Instead of searching for random, fleeting fixes, it’s best to see if you can analyze your situation and remove any major obstacles that are capable — on their own — of causing debilitating, unrelenting insomnia, the kind that occurs despite even the best of sleep hygiene habits.
Nail down your sleep hygiene:
Related Articles

Why ‘Nobody’ Believes the Mold Sufferer
If there were a battle hymn of the mold sufferer, it would be titled: “Why Does Nobody Believe Me?”

An Exercise for Dealing With Loved Ones We Disagree With
An 11-question inventory for furthering relationships.

What I Do (New: 7-15-2023)
Here’s what I’m currently doing to improve my health.

‘Sensitization’ = Environmental Illness?
An introduction to environmental sensitivities.

5 Elements of Healthy Buildings
Let’s run through five big elements of healthy buildings.

Nutrient Balancing for Insomnia
Certain nutrients are much more important for sleep than others.